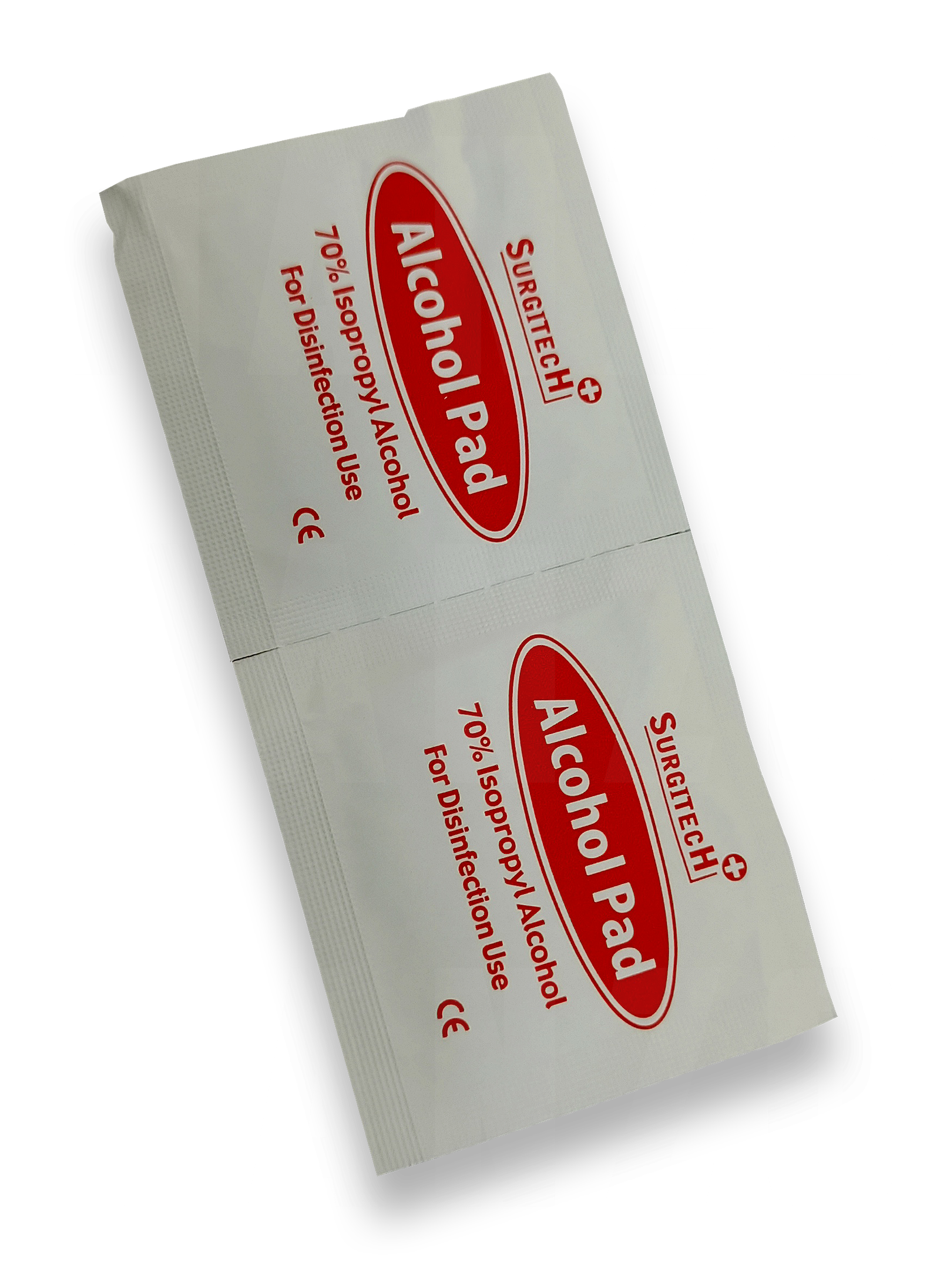
Alcohol Pad – Surgitech
₱0.99- Alcohol Pad Saturated, 70 Isopropyl Alcohol, 100 Pieces
Sterile processing and infection control are critical components of healthcare that focus on ensuring medical instruments, equipment, and environments are free from harmful microorganisms, reducing the risk of infections in patients and healthcare workers. Sterile processing involves cleaning, disinfecting, and sterilizing medical instruments, while infection control focuses on preventing the spread of infections within healthcare settings.
Sterile Processing
Sterile processing refers to the procedures used to clean, disinfect, and sterilize medical equipment to ensure it is safe for reuse. The sterile processing department (SPD), sometimes referred to as the central supply or sterile supply department, plays a vital role in maintaining patient safety.
Key Steps in Sterile Processing:
1. Decontamination:
– Instruments and equipment are thoroughly cleaned to remove blood, tissue, and other contaminants after use. This is the first step in the sterile processing workflow.
– Tools used in decontamination include enzymatic detergents, washers, ultrasonic cleaners, and manual scrubbing.
2.Inspection:
– After decontamination, instruments are carefully inspected for damage, wear, or remaining contaminants. This step ensures only fully functional and clean instruments move to the next stage.
– Visual inspections or magnification tools are often used to ensure thorough cleaning and check for signs of wear and tear.
3.Assembly and Packaging:
– Clean instruments are sorted and assembled into sets according to their use in surgeries or procedures.
– Items are packaged in sterile wraps, containers, or pouches that allow for sterilization while protecting the instruments from contamination until use.
4. Sterilization:
– The instruments are placed into sterilizers where they undergo processes such as steam sterilization (autoclaving), gas sterilization (ethylene oxide), or low-temperature sterilization (hydrogen peroxide or plasma sterilization).
– Sterilization methods are chosen based on the instrument’s material and tolerance to heat or moisture.
5. Storage:
– After sterilization, instruments are stored in sterile conditions until they are needed. Storage areas must remain clean and controlled to ensure sterility is maintained until use.
– Sterile trays and packs are labeled with expiration dates to ensure instruments are used within safe time frames.
Sterilization Methods:
– Steam Sterilization (Autoclaving): High-temperature steam under pressure kills microorganisms, including spores. It’s the most common and effective sterilization method for heat-tolerant instruments.
– Ethylene Oxide (EO) Gas Sterilization: Used for heat- or moisture-sensitive devices, this process involves exposing instruments to ethylene oxide gas, which kills microorganisms. EO is highly effective but requires lengthy aeration to remove residual gas.
– Hydrogen Peroxide Plasma Sterilization: A low-temperature method used for heat-sensitive instruments, hydrogen peroxide vapor and plasma effectively sterilize equipment without moisture.
– Dry Heat Sterilization: Used for instruments that cannot be sterilized by steam, this method involves prolonged exposure to high temperatures.
Infection Control
Infection control refers to the practices used in healthcare settings to prevent and control the spread of infections. It encompasses a wide range of strategies, from personal protective equipment (PPE) to sanitation protocols, ensuring that healthcare environments remain safe and infection risks are minimized.
Key Aspects of Infection Control:
1. Hand Hygiene:
– Proper hand hygiene is one of the most effective ways to prevent the spread of infections. Handwashing with soap and water or using alcohol-based hand sanitizers is essential in all healthcare settings.
– Healthcare workers are required to practice hand hygiene before and after patient contact, after touching potentially contaminated surfaces, and before donning gloves.
2. Personal Protective Equipment (PPE):
– PPE, including gloves, gowns, masks, face shields, and eye protection, helps protect healthcare workers from exposure to infectious agents and prevents cross-contamination between patients.
– Proper donning (putting on) and doffing (removing) procedures are crucial to avoid self-contamination.
3. Sterile Field Maintenance:
– In surgical environments or during invasive procedures, a sterile field is created to prevent infection. Maintaining this sterile field involves strict protocols to ensure that only sterilized instruments, dressings, and equipment come into contact with the patient.
– Healthcare workers must use sterile gowns and gloves and avoid any contact with non-sterile surfaces.
4. Environmental Cleaning and Disinfection:
– Hospital rooms, operating rooms, and equipment must be regularly cleaned and disinfected using EPA-approved disinfectants to remove harmful microorganisms.
– High-touch surfaces, such as bed rails, doorknobs, and medical equipment, are frequently disinfected to minimize infection risk.
5. Isolation Precautions:
– Standard Precautions: These are applied to all patients, regardless of diagnosis, and include hand hygiene, the use of PPE, and safe injection practices.
– Transmission-Based Precautions: Additional measures are taken based on the mode of transmission (e.g., airborne, droplet, contact precautions). Patients with infectious diseases may be placed in isolation rooms to prevent the spread of pathogens.
– Negative-pressure rooms are used for airborne precautions (e.g., for tuberculosis or COVID-19 patients), while contact precautions involve the use of gloves and gowns when touching the patient or their environment.
6. Waste Disposal and Sharps Management:
– Medical waste, including contaminated items like bandages, needles, and body fluids, must be disposed of according to strict biohazard protocols to avoid infection risks.
– Sharps (e.g., needles, scalpels) are disposed of in specially designed containers to prevent accidental needlestick injuries, which can spread infections.
7. Vaccination and Immunization:
– Healthcare workers are often required to receive vaccinations to protect against certain infections, such as influenza, hepatitis B, and COVID-19.
– Immunization programs also extend to patients to help prevent outbreaks of vaccine-preventable diseases.
8. Antibiotic Stewardship:
– Antibiotic stewardship programs aim to reduce the overuse and misuse of antibiotics, which can lead to the development of antibiotic-resistant bacteria. Infection control strategies help prevent infections that might otherwise require antibiotic treatment.
The Importance of Sterile Processing and Infection Control
1. Patient Safety:
– Sterile processing and infection control protocols are essential for preventing healthcare-associated infections (HAIs), which can occur in hospitals, surgical centers, and other medical facilities.
2. Compliance with Standards:
– Healthcare facilities must comply with regulations from organizations like the Centers for Disease Control and Prevention (CDC), World Health Organization (WHO), and The Joint Commission, which provide guidelines for sterilization and infection prevention.
3. Protecting Healthcare Workers:
– Infection control measures, including proper PPE use, vaccinations, and hand hygiene, protect healthcare workers from acquiring infections from patients.
4. Reducing the Spread of Disease:
– Effective infection control measures help prevent the spread of infectious diseases within healthcare settings and in the community.
Conclusion
Sterile processing and infection control are essential components of healthcare that ensure medical instruments and environments are safe for use. Proper sterilization of equipment, along with adherence to infection control protocols, protects patients, healthcare workers, and the community from potentially dangerous infections, ensuring a safe healthcare environment.
Showing 1–16 of 31 results





























